Curated from the article Safe Patient Handling and Mobility: Past and Present by Karen Egli, RN, BA, CWCN and published in Sizewise in April 2015 & updated in August 2017. The full article may be read here.
Musculoskeletal disorders (MSDs) are not a new issue. The first major nursing textbook, published in the late 1800s, spoke of a nurse’s back injury due to improper patient repositioning.¹ Today, statistics still show that the health care industry remains among the top fields suffering from MSDs. Patients who lack proper movement, lifting, and mobility are at a high risk for issues like ulcers, skin tears, pneumonia, and organ atrophy. Having appropriate Safe Patient Handling and Mobility (SPHM) standards established and in place allows for a safer work environment, raises awareness for potential safety issues, and results in an increase in patient quality outcomes.

photo by PHS Medical |
THE NEED FOR STANDARDS
It is estimated that the nursing workforce will be down by one million by the year 2020. Part of this statistic is the 12-18 percent of nurses who quit due to chronic lower back pain.³ Increasing obesity, comorbidities, and patient complexity in the acute care setting places caregivers and patients at a higher risk for injury. Recent studies find that many caregivers’ musculoskeletal injuries are the result of repetitive lifting movements (e.g. sliding/pulling a patient up in bed). These motions produce a shearing force on the spine that cause micro-tears, which weaken the spine and make it more prone to injury.(5) A 2012 study by the US Department of Labor found that health care workers suffer more injuries than those in the manufacturing and construction industry. Injuries occurring from overexertion were twice the average rate, while nursing home workers accounted for more than three times the average rate of injury.(7) SPHM standards were long overdue to ensure a safer work environment, as well as a safer healing environment for patients.
DEVELOPMENT OF SPHM STANDARDS
SPHM standards have been in development for decades. A Health and Safety Survey found that 62 percent of nurses surveyed in a sample of almost 5,000 identify musculoskeletal injuries as a top concern of their profession.² In addition, 34 percent of hospital nurses reported back, neck, and shoulder pain, and 84 percent of these respondents reported having a work-related back injury that limited their ability to move properly.(10) In 2003, the American Nurses Association (ANA) introduced the Handling with Care Campaign. Ten states were required to develop comprehensive programs in place to reduce MSDs through an increase in education regarding safe patient mobility, an increase in the use of assisted lifting and repositioning devices, and the commitment to adhere to federal and state ergonomic policies.(11) In 2011, development of official SPHM standards began, with completion in the summer of 2013 when the ANA published Safe Patient Handling and Mobility: Inter- professional National Standards Across the Care Continuum.
A SAFER SOLUTION: THE EPIDURAL POSITIONING DEVICE (EPD)
Designed by an anesthesiologist and patented in 2001, the Epidural Positioning Device positions patients correctly and comfortably by encouraging cervical, thoracic and lumbar flexion while maintaining a solid and stable position. Manually controlled chest, arm and head support ensure that patients of every body type and size can be accommodated and the spine remains immobile during epidural placement. What does this mean for the medical setting? By investing in an Epidural Positioning Device you can improve safety with standardized practice, improve risk reduction by minimizing work-related injuries, and increase patient satisfaction.
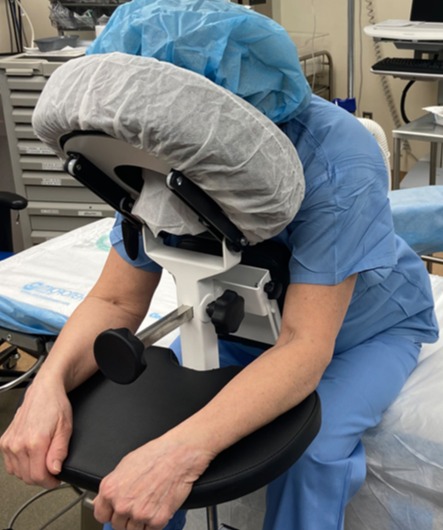
Photo by PHS Medical
CONCLUSION
SPHM standards have been needed for decades. Historically, it was considered the nurse’s fault for injuring his/her back, and standards went undeveloped as injuries went unaddressed. While we have evolved from that mode of thinking, it is critical that our knowledge and thinking continues to guide efforts to make the health care environment safe for nurses, staff, and patients. Proper training and equipment can result in a significant reduction in back injuries, aid in early mobilization of patients, and increase quality of patient care.
References:
- Hampton, Nursing: its principles and practice. Cleveland, OH: 1898, J. B. Savage. 2. American Nurses Association (2013). Safe patient handling and mobility: Interprofessional national standards. Silver Spring, MD. Nursesbooks.org, 3. Nelson, Kathleen. SPHM Annual Conference 2014. 4. Nelson, A., Baptiste, A. Evidence-Based Practices for Safe Patient Handling and Movement. Online Journal of Issues in Nursing. Vol. #9 #3, Manuscript 3. nursingworld.org/ojin/topic25/tpc25_3.htm. 5. Meier E. Ergonomic Standards and Implications for Nursing. Nursing Economics, January, 2001. Available at http://findarticles.com/p/articles/mi_m0FSW/is_1_10/ai_n18611327. 6. Marras, W. Safe Patient Handling & Mobility. Conference 2014. 7. Bureau of Labor Statistics (2011). 2010 nonfatal occupational injuries. Retrieved from http://www.bls.gov/iff/oshwc/osh/case/osch0045.pdf. 8. Centers for Disease Control and Prevention. (2013). Safe patient handling. Retrieved from http://www.cdc.gov/niosh/topics/safepatient/ 9. Moses, E. B. (Eds). (1992). The registered nurse populations: Findings from the national sample survey of registered nurse. Washington DC: Department of Health and Human Services, U.S. Public Health Service, Division of Nursing. 10. Owens, B. The magnitude of low-back problems in nursing. Western Journal of Nursing Research 1989; 11, 234-242. 11. Smedley, J., Inskip, H., Trevelyan, G., Buckle, P., Cooper, C., and Coggon, D. Risk factors for incident neck and shoulder pain in hospital nurses. Occupational & Environmental Medicine 2003; 60, 864-869. 12. American Nurses Association (2014). Safe patient handling and mobility (SPHM). Retrieved from http://www.nursingworld.org/MainMenuCategories/Policy- Advocacy/State/Legislative-Agenda-Reports/State-SafePatientHandling. 13. Fitzpatrick, M. A. (2014). Safe patient handling and mobility: A call to action. Current Topics in Safe Patient Handling and Mobility. Retrieved from www. americannursetoday.com/wp-content/uploads/2014/07/ant9-Patient-Handling- Supplement-821a.pdf. 14. Halbesleben, J.R.B., Managing Stress and Preventing Burnout in the Healthcare Workplace 2010. 15. OSHA (2015) Retrieved from https://www.osha.gov/SLTC/ergonomics/ controlhazards.html. 16. NPR (2015). At VA Hospitals, Training and Technology Reduce Nurses’ Injuries. http://www.npr.org/2015/02/25/387298633/at-va-hospitals-training-and- technology-reduce-nurses-injuries. 17. American Nurses Association. (2011) 2011 Health & safety Survey report. LCWA Research Group. 18. The Facility Guidelines Institute. (2010). Patient handling and movement assessments: A white paper.




